

Affiliations
ABSTRACT
Epithelial inclusion cysts of the conjunctiva are thin-walled, nonkeratinised epithelium-lined, benign cystic lesions. These sac-like lesions are filled with clear serous fluid with shed epithelial cells or gelatinous mucous substance. They are slowly progressive and cause cosmetic disfigurement, reduced ocular motility, and unstable tear film. Herein, a case of a 4-year child is presented with a large conjunctival inclusion cyst invading the corneal stroma and managed surgically under intraoperative Optical Coherence Tomography (iOCT) guidance. The patient was followed for one and a half years, and no recurrence was noted. To the best of our knowledge, it is one of the few reported cases of large epithelial inclusion cysts invading into stroma that was treated successfully.
Key Words: Conjunctiva, Cyst, Optical Coherence Tomography.
INTRODUCTION
Conjunctival cyst with inadvertent invasion into the cornea has been reported scarcely in literature. Implantation of conjunctival epithelial cells into corneal stroma leads to the formation of corneal inclusion cyst. These cysts can be primary (congenital) or secondary (acquired). Primary inclusion cyst forms during embryonic development due to excessive invagination of caruncular or forniceal epithelium.1 Secondary cysts develop when the surface epithelium is displaced into substantia propria following trauma, inflammation, or ocular surgeries, e.g. cataract, squint surgery, scleral buckling, pterygium excision, pars plana vitrectomy, and glaucoma drainage device insertion.2,3 The most commonest site of cyst involvement is the superior nasal bulbar conjunctiva.4 Indications of surgical intervention are vision loss, threatened visual axis, cosmetic blemish, and progressively enlarged cyst.5 Intraoperative Optical Coherence Tomography (iOCT) is a cutting-edge and revolutionary technology that provides a real-time dynamic feedback of tissue alterations during surgery and layer-by-layer dissection of the stroma.6
Herein, we describe a case of a 4-year child who presented with a large conjunctival inclusion cyst invading the corneal stroma and managed surgically under intraoperative iOCT guidance.
CASE REPORT
A 4-year male child was brought by his parents with progres-sively increasing painless swelling on the left superonasal ocular surface. The swelling progressively increased in size and displaced into the cornea. Primary complaints were discomfort and cosmetic concerns. There was no history of chronic eye rubbing, watering, redness, and history of trauma, or ocular surgery.
On ocular examination, his unaided vision in the right eye was 6/9, while in the left eye, it was perception of light. An examination under anaesthesia (EUA) revealed cystic swelling originating from superonasal fornix and encroaching almost the entire corneal stroma sparing 1-2 mm of temporal limbus from 1 to 5 o’clock (Figure 1A and 1C). Whitish specks in opalescent fluid were noticed floating within the cyst. Anterior chamber, pupil, and lenticular details were not clear. Posterior segment was not visible. The ocular examination of the right eye was unremarkable.
On iOCT of the cornea, it was well-circumscribed cystic swelling within the stroma (Figure 1B) and had no communication with the anterior chamber. On ultrasonography (USG) B-scan, lens was at normal position, and retina was flat.
Due to the involvement of visual axis, a management plan of the excision of conjunctivo-corneal cyst with or without keratoplasty under general anaesthesia (GA) was made. Informed written consent was taken from parents. Patient was draped under GA and a limbal bridal suture was inserted. Cyst was separated from the conjunctiva and tenon. Haemostasis was achieved. Fluid was aspirated and sent for cytology. Dissection was extended towards cornea.
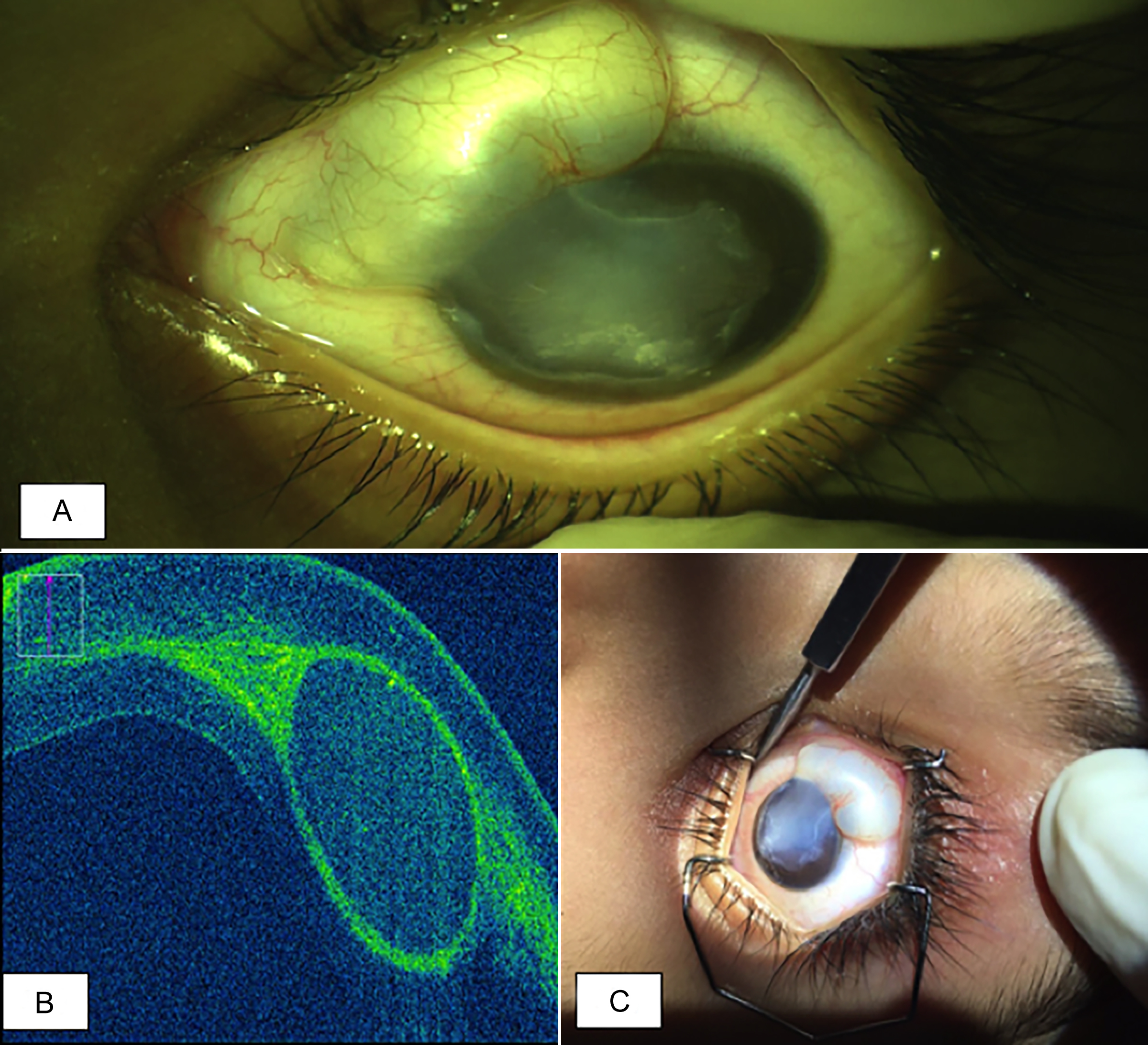 Figure 1: (A) Cyst arising from superonasal aspect on ocular surface and encroaching intra-stromally into the cornea. (B) Cyst on intraoperative optical coherence tomography. (C) The gross appearance during examination under anaesthesia.
Figure 1: (A) Cyst arising from superonasal aspect on ocular surface and encroaching intra-stromally into the cornea. (B) Cyst on intraoperative optical coherence tomography. (C) The gross appearance during examination under anaesthesia.
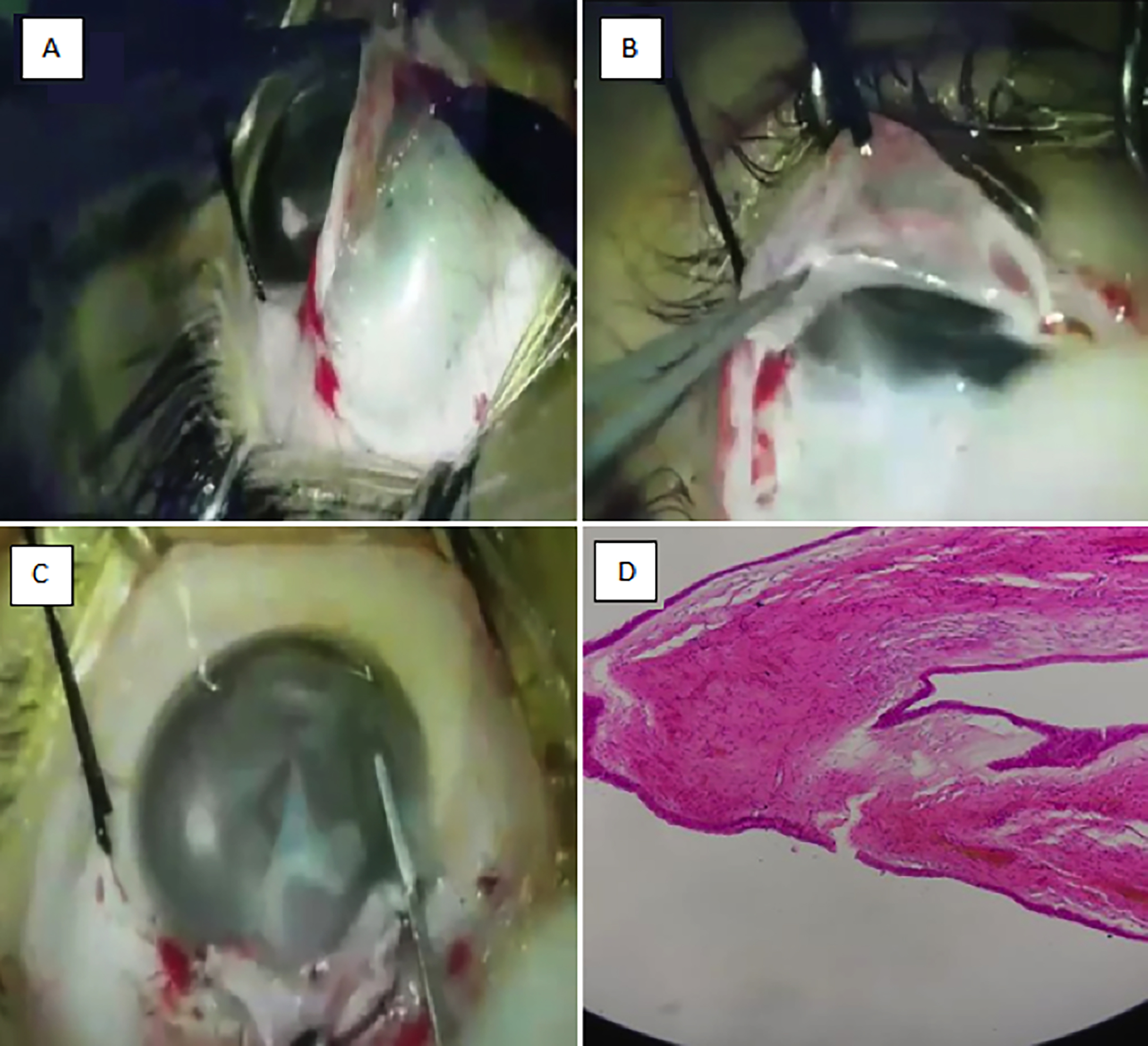 Figure 2: (A) It shows episcleral portion of the cyst, the overlying conjunctiva has been reflected. (B) It shows a deflated and dissected episcleral cyst. (C) It shows intraoperative optical coherence tomography-guided stromal dissection and removal of pieces of the cyst. (D) It shows histopathogical picture of the dissected tissue showing inclusion cyst.
Figure 2: (A) It shows episcleral portion of the cyst, the overlying conjunctiva has been reflected. (B) It shows a deflated and dissected episcleral cyst. (C) It shows intraoperative optical coherence tomography-guided stromal dissection and removal of pieces of the cyst. (D) It shows histopathogical picture of the dissected tissue showing inclusion cyst.
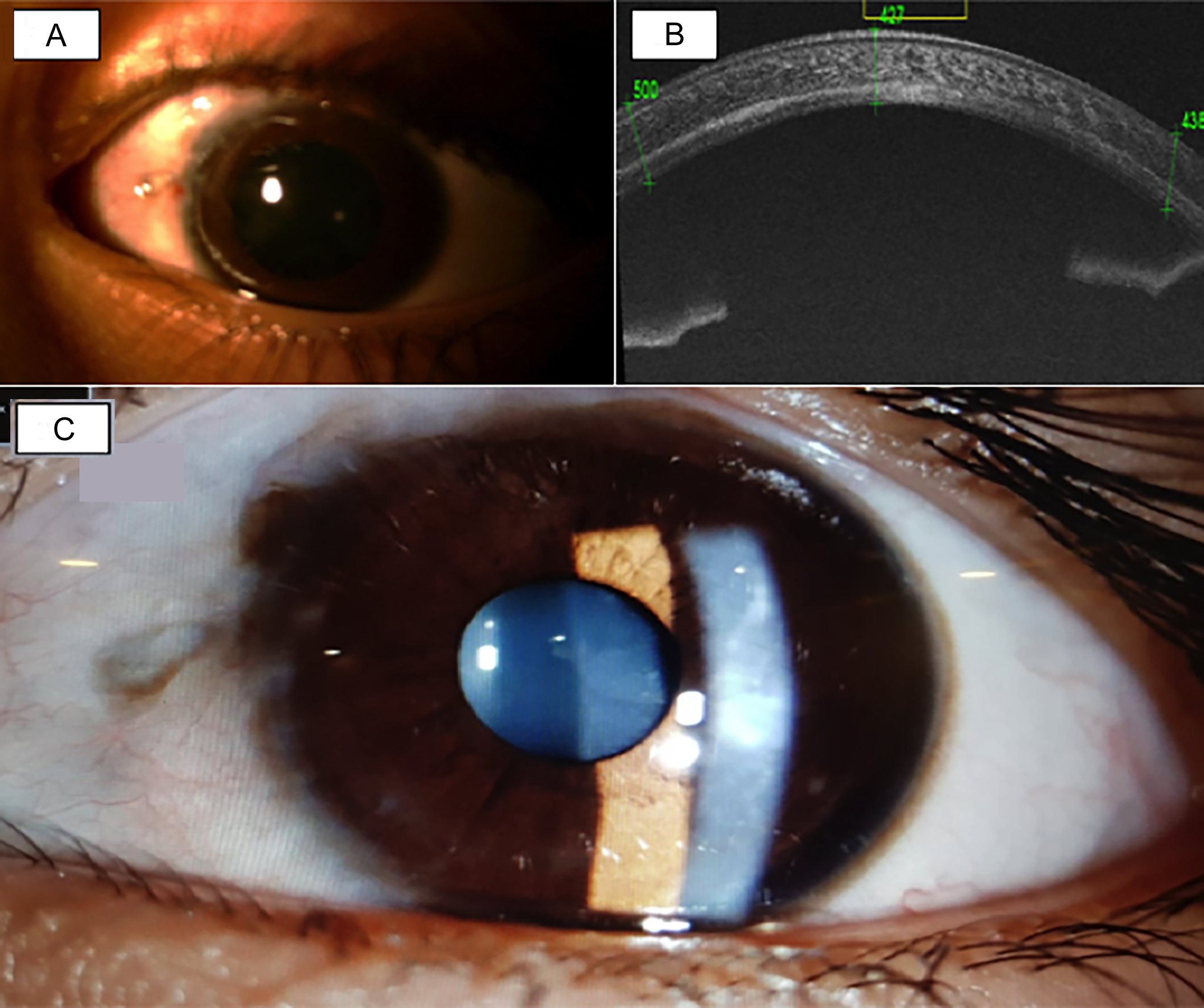 Figure 3: (A) and (B) show cornea and anterior segment on OCT at 6-month postoperatively, (C) shows picture at 1st year.
Figure 3: (A) and (B) show cornea and anterior segment on OCT at 6-month postoperatively, (C) shows picture at 1st year.
Anterior and posterior lamella of cornea were completely adherent to the cyst, so they were separated into two laminae, and the cyst was removed in pieces from the stroma. With the assistance of iOCT, direct visualisation of corneal layers was possible (Figure 2).
After removing adherent cystic epithelium and residual contents from the stroma, the corneal laminae were re-positioned and sutured from 6 to 1 o’clock. Excised stromal cyst pieces and conjunctival cyst were sent for histopathological examination that revealed benign conjunctival cyst both in the corneal stroma and the episcleral portion (Figure 2D). Aspirated fluid examination showed no malignant cells or echinococcosis parasite. Amblyopia therapy for 5-6 hours was advised as the visual axis was now clear and fundus examination was unremarkable. Monthly follow-up was advised for assessing recurrence (Figure 3A), left-eye vision and to check reverse amblyopia. At one year follow-up, the best corrected visual acuity in the right eye was 6/6 and in the left-eye was 6/38 with no further improvement. He had refractive errors of -1.00 DC×170° in the right-eye and -2.00DS/ -5.00DC×30° in the left-eye. Anterior segment OCT showed adequate corneal thickness (Figure 3B) and no recurrence (Figure 3C). Parents were counselled and amblyopia therapy was continued.
DISCUSSION
Very few reports are available on intra-stromal inclusion cysts in the published literature. In this case, the cyst had encroached into the cornea occluding the visual axis comp-letely and causing sensory deprivation amblyopia, thus necessitating the need for urgent surgical intervention.
Thatte et al. studied 40 patients with conjunctival cysts and reported that intact removal of the epithelial inclusion cyst is crucial to prevent the recurrence of the cyst.6 In the present case, we followed the child for one and a half years and found no recurrence. Bagheri et al. successfully treated 10 cases of conjunctival inclusion cysts with 10% trichloroacetic acid and reported no recurrences.7 Kotharai managed two cases of small conjunctival cysts following squint surgery with intralesional 70% isopropyl alcohol with paired injection technique.8 Neither any disinfectant nor any cytotoxic chemotherapeutic agent was used intraoperatively due to the risk of corneal toxicity and perforation.
The surgery of this corneal inclusion cyst was very chal-lenging. Keeping a corneal graft for keratoplasty in backup was very important, as there was a high risk of corneal perforation during stromal manipulation. Zare et al. advised to use penetrating or lamellar keratoplasty in recurrent corneal cysts, cysts with deep extension into the stroma, and cysts involving the visual axis.5 Gokhale treated intra-stromal cyst with 96% ethanol irrigation that recurred, which was then managed with vacuum-assisted cyst wall excision.9 In the present case, we successfully dissected and meticulously removed the cyst without landing into any complications and salvaged corneal tissue. Postoperative follow-up for assessing recurrence and to prevent amblyopia in children is a vital part of patient-care in such cases.
The conjunctival inclusion cyst threatening the visual axis should be timely managed surgically to prevent sensory deprivation amblyopia. Recurrence is inevitable if there is no careful removal of the cyst matter. iOCT is an emerging tool in performing manual lamellar dissection in corneal surgeries.
PATIENT’S CONSENT:
Informed written consent was taken from the patient’s parents.
COMPETING INTEREST:
The authors had no conflicts of interest to declare.
AUTHORS’ CONTRIBUTION:
TAJ: Conception and design of the work.
MQ: Acquisition and drafting of the work.
AF: Editing and revising the manuscript critically.
All authors read and approved the final version of the manu-script to be published.
REFERENCES